Top 5 Cardiometabolic Health Topics You Can’t Miss at the 14th Annual CMHC
Alarmingly, recent statistics indicate that over one-third of the population has at least one cardiometabolic risk factor, ranging from dyslipidemia and hypertension to diabetes and cardiovascular disease. In the time of a cardiometabolic public health crisis, it is more important than ever for clinicians to equip themselves with the latest therapeutic strategies and protocols in order to prevent, treat, and manage disease. Delivering optimal patient care and enhancing health outcomes requires medical professionals to stay up-to-date on developments and advances in cardiometabolic health through continuing medical education.
With an emphasis on hands-on, directly applicable education, the 14th Annual Cardiometabolic Health Congress provides an opportunity for healthcare practitioners to familiarize themselves with developments in cardiometabolic health. A top-tier multi-disciplinary conference led by a panel of influential leaders, The Cardiometabolic Event of the Year™ will review the most recent and relevant research and delve into strategies for safely and effectively merging new protocols into clinical practice. From the rapidly emerging role of big data in cardiometabolic medicine to the advances and challenges in hyperkalemia management, attendees will have the opportunity to explore the most clinically current topics in the field through a series of expert-led sessions curated to provide a comprehensive understanding of the latest updates in the field.
The Role of Big Data in Cardiometabolic Health
The prevalence of digital technology in the medical industry shows no signs of slowing down. Increasingly, healthcare practitioners are being encouraged by hospitals and insurance companies to adopt new technologies. Radiologists, cardiologists, and pulmonologists are now more reliant on automated high dimensional image processing algorithms and other artificial intelligence technologies, while clinicians of all specialties will soon see the effects of the digital revolution in practice. Although controversial, forthcoming digital technology has the potential to greatly enhance the practice of modern medicine.
Improving population health outcomes can be made significantly more achievable using these latest advances in medical technology. For example, by replacing sparse, sporadically collected patient datasets with continuous data and vital parameters gathered from wearable medical technology, practitioners can gain greater insight into real-time patient health to improve diagnostic and treatment strategies. A comprehensive understanding of big data, machine learning, and other digital advancements can better equip clinicians to safely and effectively integrate novel health technologies into their practice.
Whether looking to learn more about the implications of big data on the cardiometabolic field or simply beginning to understand the basics of machine learning in medicine, the expertly curated Cardiometabolic Technology Summit allows participants the opportunity to familiarize themselves with an array of digital advancements and their practical solutions. For clinicians wanting to stay clinically current and educated on the growing role of big data in the cardiometabolic field, the one-day pre-conference event will review the latest during the Introduction to Big Data and Its Role in Cardiometabolic Health session on Thursday, October 10th. Spotlighting the newest medical devices, technological advancements, and more, the symposium is designed to equip attendees with digital health strategies and techniques to seamlessly integrate into patient care.
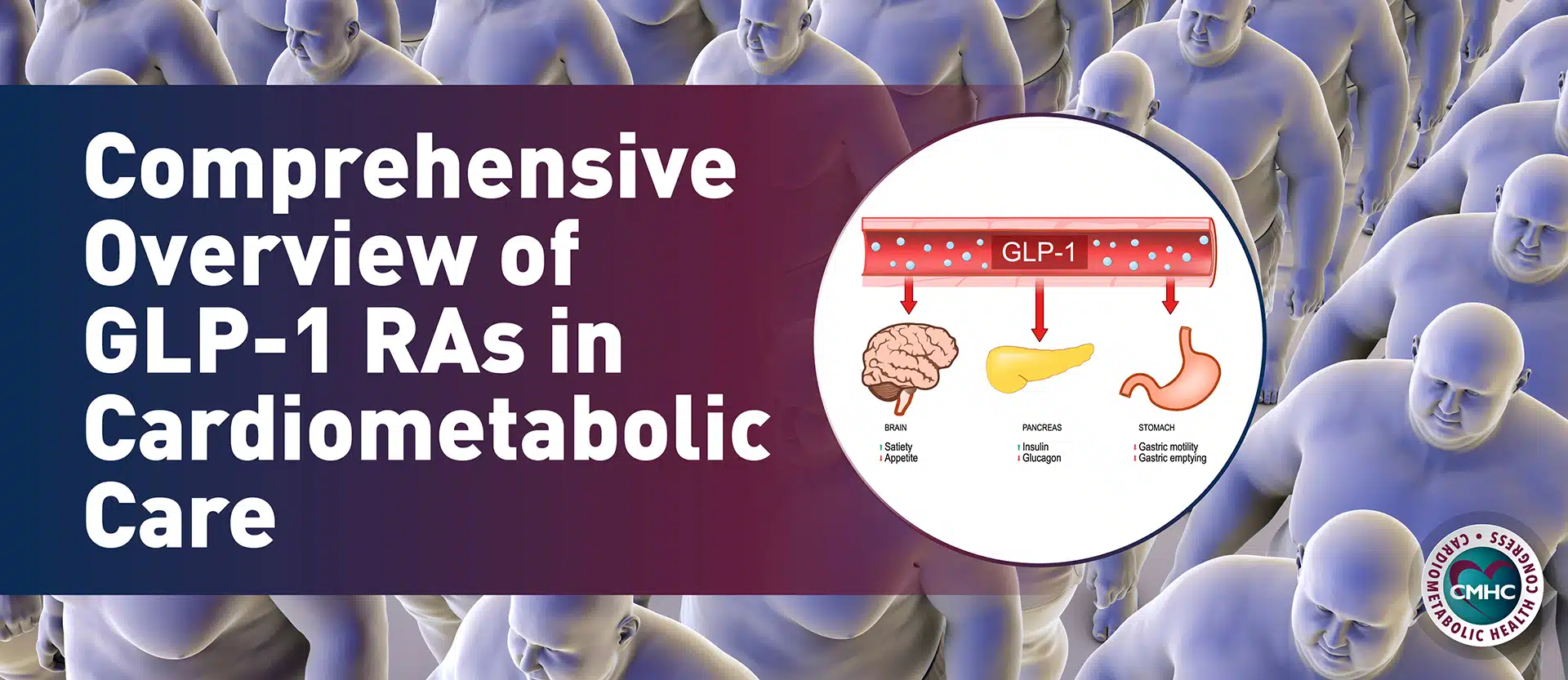
Reducing Cardiovascular Risk in T2DM Patients
The underlying links between type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD) reveal the interplay of several lifestyle risk factors, including nutritional patterns, physical activity, body weight and BMI. Not only do patients with type 2 diabetes mellitus (T2DM) experience a doubled mortality risk, but they also face a 10-fold increase in hospitalization rate for coronary heart disease. As more than one-third of U.S. adults have prediabetes and are at risk of developing T2DM, and approximately 12% of adult Americans currently have diabetes, there is an urgent need for the development of comprehensive prevention strategies aimed at reducing the risk of cardiovascular events in these patients. The latest guidelines for CVD prevention from the American College of Cardiology (ACC) and the American Heart Association (AHA) include specific recommendations for T2DM patients, which target four specific areas: statin therapy, nutrition, physical activity, and the use of antihyperglycemic agents. Both sodium-glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1RAs) have been found to effectively lower blood pressure, reducing the number of CVD events in adults with T2DM. Trials that reveal the efficacy of pharmacologic treatment provide valuable practice-changing insights that encourage shifting the focus of T2DM management to include CV risk management and prevention.
To access the latest information on outcome trials, how to interpret and implement their results, and how to optimize therapeutic strategies for patients with T2DM and cardiovascular risk attend the Reducing Cardiovascular Risk: A Paradigm Shift in T2DM Management CME Lunch Symposium on Friday, October 11th chaired by Dr. Robert Eckel.
Challenges and Advancements in Hyperkalemia Management
Defined as a serum potassium concentration of >5.5 mEq/L in adults, hyperkalemia is a common metabolic disorder associated with an increased risk of mortality. The condition is frequently diagnosed and recurs in patients who have a history of heart failure (HF), chronic kidney disease (CKD), and hypertension. Patients with comorbid illnesses, those who take renin-engiotensin-aldosterone system (RAAS) inhibitors, beta-blockers, non-steroidal anti-inflammatory drugs (NSAIDs), or other medications may be at risk of developing elevated potassium levels and have an increased chronic risk for hyperkalemia.
Until recently, management strategies for hyperkalemia were lacking with no long-term outcome data to inform care. The latest advancements in hyperkalemia management include novel potassium-binding agents for improved long-term management of the condition, which could greatly diminish the burden of hyperkalemia in cardiometabolic patients. Current clinical evidence reveals the necessary guidelines associated with these drugs to help clinicians optimize medical therapy for hyperkalemic patients with HF and CKD.
To learn how to identify patients at risk for hyperkalemia based on risk factors, interpret the efficacy and safety of current and new treatment options, and develop appropriate treatment strategies for patients with HF and CKD, attend The Potassium Dilemma in HF and CKD: Challenges and Advancements in the Management of Hyperkalemia CME Breakfast Symposium on Saturday, October 12th led by Dr. George Bakris.
The Latest in Iron Repletion Therapy
Approximately 3 billion people around the world have iron deficiency (ID), and countless potential causes exist, including pregnancy, gastric bypass operations, multiple surgical procedures, and colorectal cancer. At the same time, there is a growing awareness of the prevalence of iron deficiency in patients with heart failure – in over 30% to 50% of patients with stable chronic HF – which greatly affects outcomes despite the latest advances in HF management.
Recent and ongoing trials of iron repletion therapy in patients with HF reveal promising results in improving condition management and reducing HF hospitalizations, highlighting the importance of diagnosis and proper care of this common comorbidity. The latest updates to established HF treatment guidelines emphasize ID recognition and treatment – which can vary from oral to intravenous iron formulations based on individual patient needs.
Healthcare practitioners looking to improve their ability to diagnose and describe the prevalence of ID in HF, its impact on patient outcomes and quality of life, and develop individual treatment regimens can attend the Advances in Iron Repletion Therapy: Addressing the Burden of Iron Deficiency in Patients with Heart Failure to Improve Outcomes and Quality of Life CME Lunch Symposium chaired by Dr. Peter McCullough on Saturday, October 12th.
Diabetic Kidney Disease Progression
One of the most common complications of diabetes, diabetic kidney disease (DKD) affects up to half of all diabetic patients, leading to increased morbidity and mortality. Despite improvements in glycemic control strategies and renin-angiotensin-aldosterone system (RAAS) inhibitor therapies, the unmet need to reduce diabetic kidney disease progression to kidney failure remains. With a growing understanding of disease pathophysiology, research has opened up the possibility of novel treatment methods – such as mineralocorticoid receptor antagonism – which have the potential to greatly improve patient outcomes. Recent and forthcoming clinical trials demonstrate the efficacy of non-steroidal mineralocorticoid receptor antagonists (MRAs) in halting disease progression.
During Session 1 of the Cardiometabolic Health Congress, experts will review the most recent clinical trial data with MRAs in DKD, provide an overview of the underlying pathophysiology, and outline methods for identifying at-risk patients according to evidence-based guidelines. To learn more about current and emerging DKD treatments, participants can attend the Addressing the Unmet Need of Diabetic Kidney Disease Progression: Beyond SGLT-2 Inhibitors and GLP-1 Ras CME Lunch Symposium on Friday, October 11th led by Dr. George Bakris.
The 14th Annual Cardiometabolic Health Congress
Serving as the go-to forum for health practitioners looking to stay clinically current and educated in their field, the 14th Annual Cardiometabolic Health Congress is the largest multidisciplinary conference focused on the management, prevention, and treatment of cardiovascular and metabolic disease. During the 3 ½ days of expertly curated sessions chaired by the nation’s leading experts, attendees will obtain a comprehensive understanding of the latest advancement in cardiometabolic care alongside directly applicable solutions to seamlessly integrate into their clinical practice.
Join hundreds of other leading medical professionals and influential experts in Chicago between October 10 – 13th at the cardiometabolic event of the year by registering for the 14th Annual Cardiometabolic Health Congress today.