The not-so-sudden rise of weight loss ”wonder” drugs for T2D and obesity
This World Obesity Day, March 4, 2024, weight loss drugs dominate discussions and raise new questions for clinicians. Glucagon-like peptide-1 (GLP-1) receptor agonists (RAs) have been used to treat type 2 diabetes (T2D) since the approval of Byetta (exenatide) in 2005. In the last decade, several more medications in this class have been approved for use in T2D and obesity. However, over the past year,
social media, celebrity testimonials, and national shortages brought GLP-1 RAs for weight loss into the limelight and skyrocketed demand.
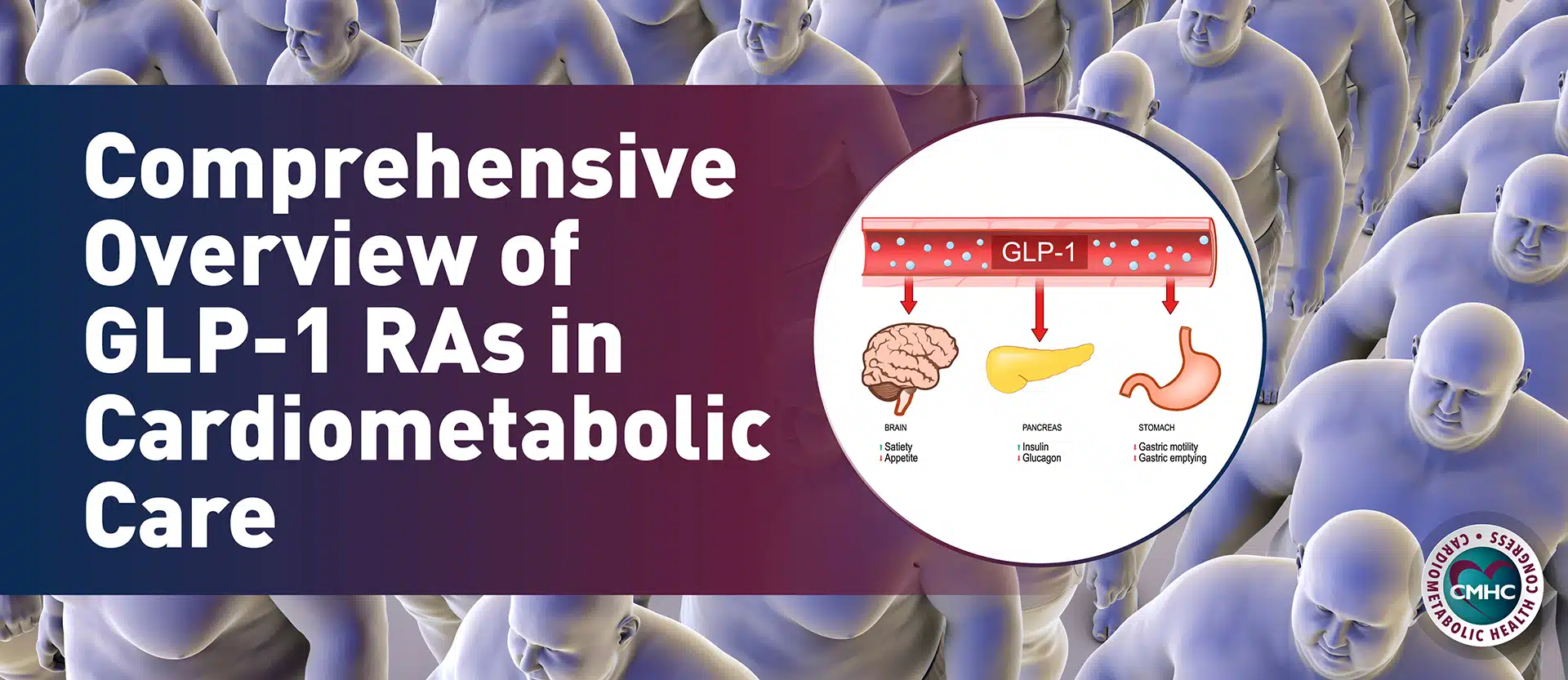
GLP-1 RAs mimic our body’s natural GLP-1. Unlike natural GLP-1, which breaks down in 1-2 minutes, the modified peptide has a longer half-life, ranging from hours to days. GLP-1 RAs augment insulin secretion after meals and inhibit glucagon production from pancreatic alpha cells at hyper- or euglycemia.
GLP-1 RAs Hold Promising Potential for Reduction of Cardiometabolic Risk Factors
GLP-1 RAs have proven potent for the management of diabetes and have been linked to
additional benefits:
Brain: Appetite suppression, nerve protection, and decreased neuroinflammation
Heart: Decreased blood pressure (systolic and diastolic), reduced total cholesterol levels, lowered endothelial dysfunction, and increased heart rate
Liver: Decreased glucose production
Pancreas: Increased insulin secretion, decreased glucagon secretion, B islet cell proliferation
GI Tract: Decreased gastric emptying
Because these drugs cause weight loss, it is not clear whether the GLP-1 RAs or the weight loss reduces cardiometabolic risks.
Approved GLP-1 RAs: Indications and Administration
These GLP-1 RA drugs are generally injected weekly or daily. Providers should note different dosing for glycemic control and/or obesity. Furthermore, the drugs are marketed under different names depending on their use case.
- Dulaglutide (Trulicity) (injection weekly) – Type 2 Diabetes
- Exenatide extended-release (Bydureon bcise) (injection weekly) – Type 2 Diabetes
- Exenatide (Byetta) (injection twice daily) – Type 2 Diabetes
- Semaglutide (Ozempic) (injection weekly) – Type 2 Diabetes
- Liraglutide (Victoza, Saxenda) (injection daily) – Obesity and Type 2 Diabetes, Respectively
- Lixisenatide (Adlyxin) (injection daily) – Type 2 Diabetes
- Semaglutide (Rybelsus) (taken by mouth once daily) – Obesity
- Semaglutide (Wegovy) (injection weekly) – Obesity
- Tirzepatide* (Mounjaro, Zepbound)(injection weekly) – Type 2 Diabetes and Obesity, Respectively
*Tirzepatide is a dual gastric inhibitory polypeptide (GIP) receptor and GLP-1 RA
View the FDA’s up-to-date list of approved GLP-1 RAs
Cardiovascular Risk Reduction Benefits of GLP-1 RAs for Patients with T2D
Those with T2D are
2 to 4 times more likely to develop cardiovascular disease (CVD) than those without T2D. CVD includes heart disease, heart failure, stroke, and peripheral arterial disease.
The good news: in addition to enhanced glycemic control and weight loss, c
ardiovascular outcomes trials (CVOT) with GLP-1 RAs suggest a positive impact on several cardiovascular risk factors for patients with T2D. These studies demonstrate a myriad of positive impacts: weight loss, reduced blood pressure, and reduced blood lipid levels. Furthermore, the stimulation of the endothelium, results in nitric oxide increases, and oxidative stress lowers for antiatherogenic and anti-inflammatory effects.
Remarkable, compared to placebo, studies over the last decade have shown GLP-1 RAs to
reduce MACE and other adverse cardiovascular events, like HF. As a result, we have seen changes in recommendations for these GLP-1s from second-line to first-line treatment in the
ADA Standards of Care in Diabetes – 2023 and updates to the
ACC 2020 Guidelines for Novel Cardiovascular Risk Reduction in Patients with T2D.
Cardiovascular benefits may be largely independent of glucose-lowering.
The next step is to dissect what is causing the reduction of cardiometabolic risk factors. It is going to be important to pull apart whether it is obesity management or direct cellular pathways—independent of glucose-lowering—leading to a positive impact on these cardiovascular risk factors.
Cardiovascular Risk Reduction Benefits of GLP-1 RAs for Your Patients With Obesity, Without T2D
One of the most pressing issues of our modern day is the obesity epidemic. At least 35% of US adults are obese and at
high risk for cardiovascular disease. How can we prevent adverse cardiovascular events in this growing population?
Enter GLP-1 RAs for obesity management and cardiovascular risk reduction. These drugs produce weight loss results previously only seen in bariatric surgery—
15-20% average weight loss!
Moreover, there is an extension of this benefit for people with diabetes found in studies of those with obesity without T2D. These studies looked at GLP1-RAs in those with obesity and other comorbidities, without T2D, at weight loss doses. Studies showed a remarkable effect on people with obesity:
The SELECT Trial found that MACE (major adverse CVD event) risk was reduced by 20% in adults with obesity without T2D in the group taking semaglutide.
STEP-HFpEF trial found substantial improvement of HF symptoms in patients with HFpeEF and obesity. Those in the semaglutide treatment group experienced about 11% greater weight loss than the placebo group, reduced inflammation, and improved physical limitations.
With a coming pipeline of weight loss drugs, this is a watershed moment. To get it right, we must look at pharmacological interventions within the context of longstanding weight loss options, like bariatric surgery. The same mental health issues we see with bariatric surgery, we’re going to see in psychological weight agents. And since obesity is chronic,
weight regains are shown to occur when stopping the medication.
When used for weight loss, we need established guidelines and comprehensive care that support the whole patient. Through strategic partnerships, we can learn from
bariatric surgery centers of excellence models: quality control, tracking results, and mental health, dietary, and physical activity counseling to achieve optimal clinical use and better outcomes for patients.
The Takeaway
Unfortunately,
few patients are being prescribed these life-saving drugs for diabetes management and reduced cardiovascular risk, possibly due to uncertainties of dosing, lack of knowledge of the CVOTs, clinical inertia, high costs, and tolerability. Clinicians need more resources like this to make informed decisions on these powerful drugs.
On the other hand, there has been a sharp uptick in prescriptions of GLP-1 RAs for weight loss with little oversight. This demands a structured, comprehensive program, fellowship training, and high-volume centers for safe and effective medical weight loss.
It remains unclear if the benefits are from the drug itself or weight loss. We need further research to understand the full potential of GLP-1 RAs and all the intricacies of their MOA for optimal clinical use.
As your go-to resource for cardiometabolic risk reduction, follow CMHC for the latest news, research, and innovations to advance your career and practice!