In March of this year, the American College of Physicians (ACP) issued a guidance statement on HbA1c targets for adults with type 2 diabetes (T2D), which have been the subject of debates and discussions in the medical community. At the center of this debate is ACP’s recommendation for a target HbA1c goal between 7-8% to maintain optimal glucose control, which is higher than what’s recommended by the American Diabetes Association (ADA) or the American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology (ACE).
ADA recommends a goal of <7% for HbA1c, even advocating more stringent goals (such as <6.5%) for certain patients with a low risk of hypoglycemia. The AACE/ACE guidelines recommend keeping glycated hemoglobin levels at ≤ 6.5% for most patients with low-risk of side effects.
The statement from ACP also recommends the individualization of T2D therapy, deintensification of therapy for patients that achieve HbA1c levels of less than 6.5%, and controlling symptoms rather than focusing on specific HbA1c goals in patients with a life expectancy of less than 10 years (such as patients aged 80 or older, that reside in a nursing home, or with chronic conditions – including dementia, cancer, end-stage kidney disease, severe COPD, or congestive heart failure). One of the main ideas behind this statement is to balance the benefits of lowering blood glucose with potential risks, such as important side effects (like hypoglycemia and weight gain), costs, and overall patient burden.
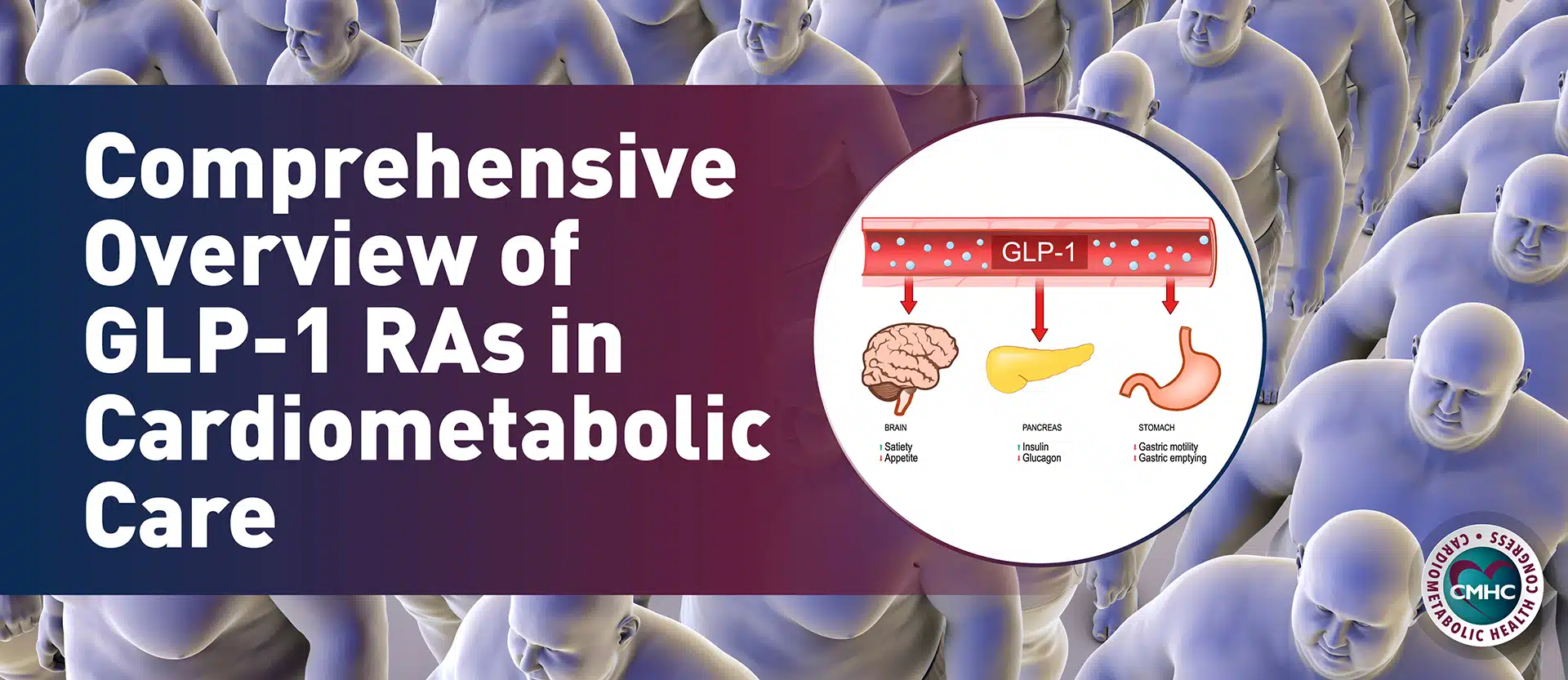
In response, ADA issued its own statement in which it disagrees with ACP’s recommended HbA1c goal of 7-8%. “Based on the evidence from the ACCORD, ADVANCE, VADT, and UKDPS trials, the ADA recommends that a goal of <7% is necessary to minimize the long-term complications of T2D”, they state in this document. Furthermore, ADA is concerned over the fact that newer anti-hyperglycemic medications, such as GLP-1 receptor agonists and SGLT-2 inhibitors, which have demonstrated favorable outcomes on hypoglycemia, weight gain, and cardiovascular disease in type 2 diabetics, are not considered in ACP’s statement. In addition, ADA doesn’t agree with general idea of deintensification of therapy for patients that achieve HbA1c targets lower than 6.5%, especially if they don’t have a history or risk of hypoglycemia.
However, even with these disagreements, there are several areas of overlap between ACP and ADA guidelines. For example, both guidelines agree that less stringent HbA1c targets may be more appropriate in patients with severe chronic comorbidities, cardiovascular disease, risk of hypoglycemia, or long-standing T2D. Additionally, deintensification or simplification of complex regimens to reduce the risk of hypoglycemia is advised in both guidelines, although disagreements remain about the cutoff HbA1c value. Focusing on symptoms rather than HbA1c values in older adults or people with short life expectancy is another area of overlap, however, the ADA does not agree with generalizing this view to anyone over the age of 80, considering the increased life expectancy in this age group. Most importantly, both associations agree that the key to optimizing glycemic control is the individualization of therapy by tailoring treatment to accommodate the specific needs and characteristics of each patient. While establishing relevant HbA1c goals is important, balancing the risk-benefit profile of pharmacotherapies with patient-level factors is key to minimizing the long-term complications of T2D, and clinicians should always use their best judgment to guide therapeutic decisions.
References
Qaseem, Amir, et al. “Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians.” Annals of Internal Medicine 168.8 (2018): 569-576.
Arlington, Virginia. “American Diabetes Association deeply concerned about new guidance from American College of Physicians regarding blood glucose targets for people with type 2 diabetes.” March 8, 2018, available at http://www.diabetes.org/newsroom/press-releases/2018/ada-acp-guidance-response.html, accessed April 30, 2018.