Long considered a guiding beacon for diabetes care, the annual Standards of Care in Diabetes – 2023 contains updated guidance for clinicians who care for the estimated 100 million patients in the U.S. with prediabetes or diabetes. New guidelines from the updated document include current clinical practice recommendations intended to optimize components of disease management, general treatment goals and guidelines, and tools to evaluate care quality. Members of the ADA’s multidisciplinary expert committee, which includes Cardiometabolic Health Congress (CMHC) faculty member Grazia Aleppo, MD, are responsible for updating these standards. New recommendations encompass obesity, hypertension, heart failure medication, social determinants of health, and lipid management.
A new set of guidelines set forth by the American Diabetes Association (ADA) in 2023 have been long-awaited by clinicians. Representatives of the ADA’s Professional Practice Committee (PPC) – responsible for updating the standards – explain that only recently did the field of study garner enough evidence to stake ground on many of these important new recommendations. The agency’s 2023 standards include lower thresholds for cholesterol and blood pressure, new confidence in recommending certain classes of drugs for renal and cardiovascular protection, and a call for physicians to lean on the entire spectrum of health providers in overcoming barriers to effective diabetes care.
The annual Standards of Care is a living document, which has been updated annually since 1989. The 2023 version contains more than 100 updated recommendations highlighting new advances in pharmacologic approaches to glycemic treatment, more aggressive lipid and blood pressure targets, patient-first language and strategies to overcome social determinants of health.
New 2023 hypertension and lipid targets
In the 2012 ADA Standards of Care, the easing of the systolic blood pressure target to 140 mmHg for patients with diabetes caused controversy among experts. As noted by members of this year’s PPC, the 2023 definition of hypertension in people with diabetes “is ≥ 130 mmHg systolic or ≥ 80 mmHg diastolic blood pressure, repeated on two measurements at different times.” In individuals with established cardiovascular disease, hypertension can be diagnosed “with just one measurement of ≥ 180/110 mmHg.” The goal of treatment is now less than 130/80 mmHg if it can be reached safely.
For low-density lipoprotein (LDL) cholesterol levels in patients with diabetes, the ADA recommends now a target of less than 70 mg/dL or no greater than 55 mg/dL, depending on the individual’s cardiovascular risk. The 2023 standards also have new therapeutic lipid targets. For people with diabetes aged 40-75 years at increased cardiovascular risk, including those with one or more atherosclerotic risk factors, high-intensity statin therapy is recommended to reduce LDL cholesterol by 50% or more from baseline and to a target of less than 70 mg/dL, in contrast to the previous target of 100 mg/dL. To achieve that goal, the document advises “adding ezetimibe or a PCSK9 inhibitor to maximally tolerated statin therapy.”
Focus on weight loss and cardiorenal risk reduction
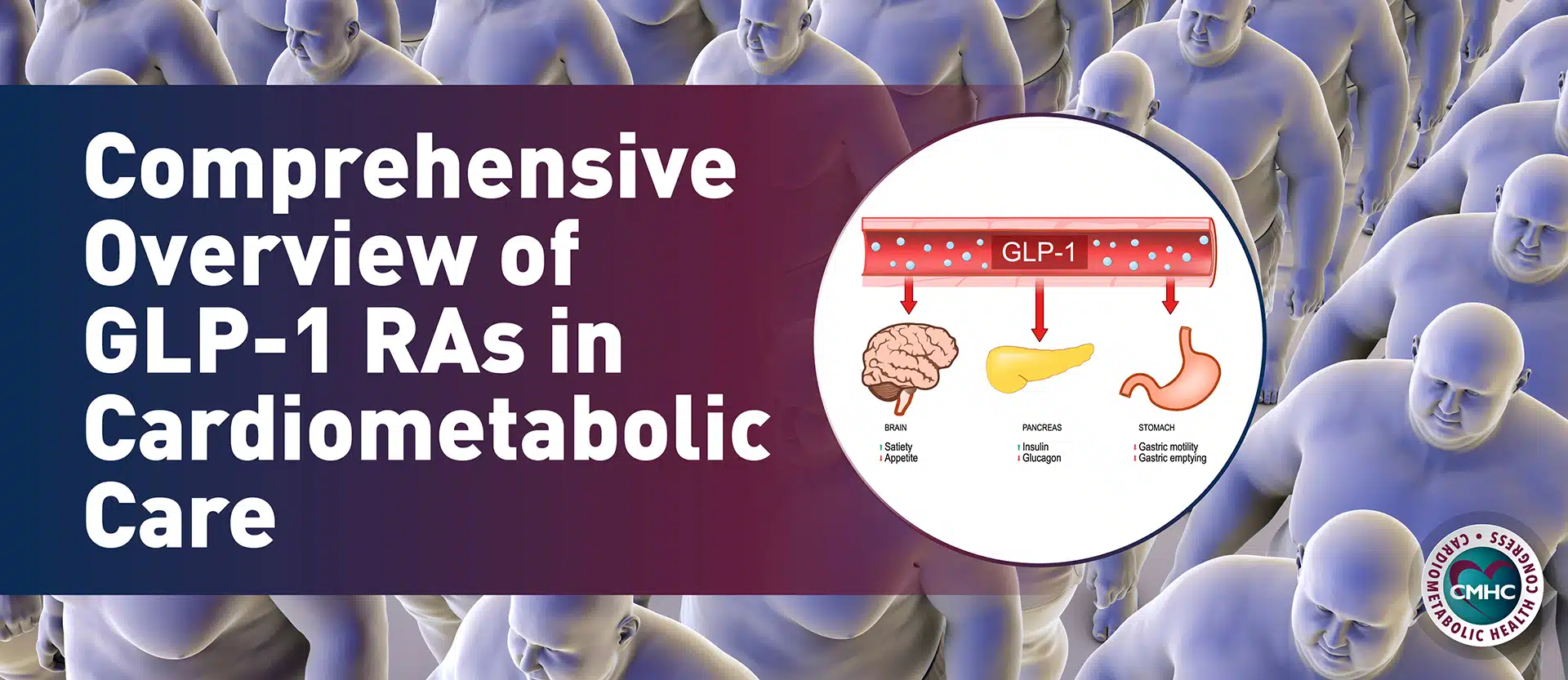
As it pertains to the management of type 2 diabetes, the ADA has emphasized an increased focus on cardiorenal risk reduction and weight management in the Standards of Care in Diabetes – 2023. Tools and therapies focus on weight loss and cardiorenal risk reduction in diabetes from a perspective other than simple glucose control. For people with diabetes aged 40-75 who have established cardiovascular disease, treatment with high-intensity statins is recommended with the target of a 50% or greater reduction from baseline and an LDL cholesterol level of 55 mg/dL or lower, in contrast to the previous 70 mg/dL.As it has for the past 6 years, the section on cardiovascular disease and risk management is also endorsed by the American College of Cardiology.
Another new recommendation from the ADA based on recent trial data is the use of sodium–glucose cotransporter 2 (SGLT2) inhibitors in people with diabetes and heart failure. Additional emphasis on supporting weight loss of up to 15% with the new twincretin tirzepatide (Mounjaro) — approved by the FDA in May 2022 for type 2 diabetes — has been added as a glucose-lowering drug with weight-loss potential.
Community health workers
New guidance also recommends using community health workers to support the management of diabetes and cardiovascular risk factors, particularly in underserved areas and health systems. Nonphysician professionals can assist with screening for food insecurity, another new recommendation. “We talk about screening for food insecurity and tools to use. That shouldn’t be something only dieticians do.”Clinicians are urged to partner with community health workers, who can help identify food insecurity and point patients and providers toward tools to screen for and address this social detriment to healthy outcomes. Community health workers can be a link to help people navigate and engage with the health system for better outcomes.”
Key takeaway
The newly published Standards of Care in Diabetes – 2023 includes recommendations for lower hypertension and lipid thresholds; a fresh emphasis on sleep, weight loss, and physical activity; using social determinants of health to inform care design and delivery; and the use of tirzepatide and finerenone based on expanded FDA approvals.
Watch Dr. Aleppo discuss the use continuous glucose monitoring in this episode of the Cardiometabolic Beat Podcast:
Resource: