Type 2 diabetes mellitus (T2DM) affects approximately 28 million people in the United States and is characterized by hyperglycemia due to insulin resistance and impaired β-cell function. Its prevalence has almost doubled in the last two decades and diabetes costs the economy $245 billion annually; with most of these costs attributed to T2DM. The rapid increase in both the prevalence and associated healthcare costs underscores the need for optimizing treatment, as several pharmacological agents for T2DM are currently approved, with many more in development. Due to the progressive nature of T2DM, early initiation of combination therapy has been proposed as an approach to achieve better preservation of β-cell function.
The Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT) study was a randomized trial to evaluate the efficacy and safety of initial triple combination therapy (metformin/pioglitazone/exenatide) compared to a conventional sequential therapy (metformin, followed by sequential add-on therapy of a sulfonylurea and basal insulin) in achieving glycemic control in T2DM patients. The original results from the EDICT study, published in 2015, demonstrated that early combination therapy in recently-diagnosed (<2 years) patients led to a greater reduction in HbA1c levels compared to conventional therapy, including a 1.2 kg mean weight loss (as compared to a 4.1 kg weight gain with conventional therapy) during a follow-up time of 24 months.1 A 6-year follow-up of this study was recently presented at the 2018 American Diabetes Association in Orlando, FL. In this follow-up, subjects that received initial triple therapy experienced significantly greater reductions in HbA1c compared to conventional therapy (mean HbA1c of 5.8% vs. 6.7%, p<0.001), with more patients achieving target HbA1c levels (<6.5%) in the triple therapy group (52%) compared to conventional therapy (25%).2 In addition, patients on initial triple therapy had improved β-cell function, less episodes of hypoglycemia, and weight loss. Progression of carotid intima media thickness, a measure of subclinical atherosclerosis, was also reduced by 50% in patients receiving triple therapy.2
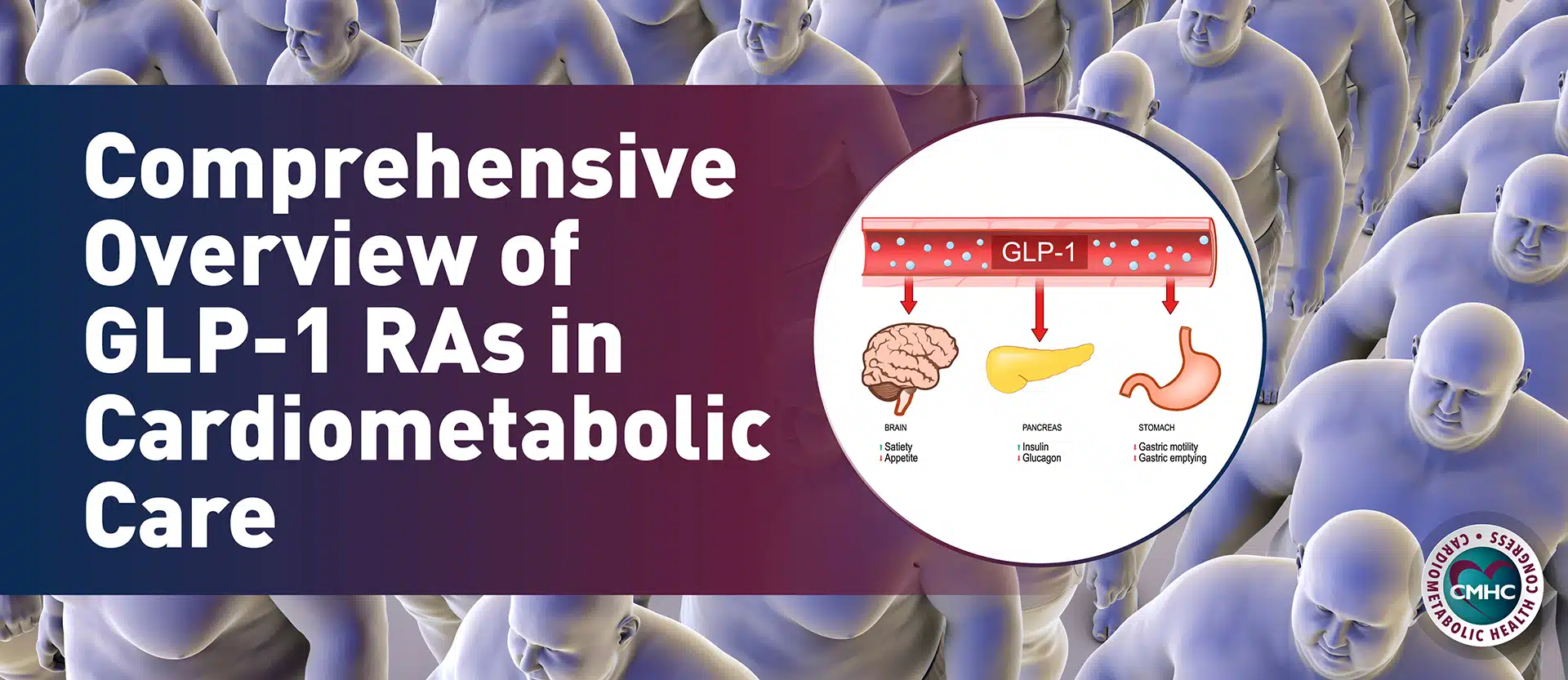
This study shows that initial combination therapy to aggressively lower HbA1c may be beneficial in the management of diabetes compared to the current sequential add-on therapy. This approach may have benefits in combating the clinical inertia in T2DM treatment, leading to positive effects on β-cell function and a greater proportion of patients achieving glycemic targets. The approval of several new agents with more favorable safety profiles, including GLP-1 RAs, SGLT-2 inhibitors, new-generation basal insulins, prandial insulins, and fixed-ratio GLP-1 RA/basal insulin combinations may further facilitate early intensification of therapy in T2DM. However, the choice of initial combination therapy compared to conventional sequential therapy may not be suitable to every patient and individualization is key.
References
1. Abdul‐Ghani, M. A., et al. “Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add‐on therapy in subjects with new‐onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): a randomized trial.” Diabetes, Obesity and Metabolism 17.3 (2015): 268-275.
2. Abdul‐Ghani, M.A., et al. “Durable HbA1c Reduction with Initial Combination Therapy with Metformin/Pioglitazone/Exenatide in Subjects with New-Onset Diabetes—Six-Year Follow-Up of the EDICT Study.” (2018): 123-OR.