The cardiorenal metabolic education continued on Thursday, Oct. 19, 2023, when the 18th Annual Cardiometabolic Health Congress (CMHC) launched its second day of sessions at the Boston Park Plaza. Attendees enjoyed sessions on emerging evidence for new agents in cardiovascular disease and obesity, a keynote address exploring social determinants of health, and the influence of modifiable lifestyle factors like sleep and physical activity on cardiorenal metabolic health.
Opening Remarks, FDA Updates and Late Breaking Trials
The second day of the 18th Annual CMHC, Social Determinants and Digital Advances in Cardiorenal Metabolic Health, began with many attendees’ favorite session on the newest evidence and approvals in hypertension, lipids, diabetes, obesity and atherosclerosis. Christie M. Ballantyne, MD, welcomed his colleagues and fellow CMHC Chairpersons to the stage to present the most recent advances in their areas of expertise.
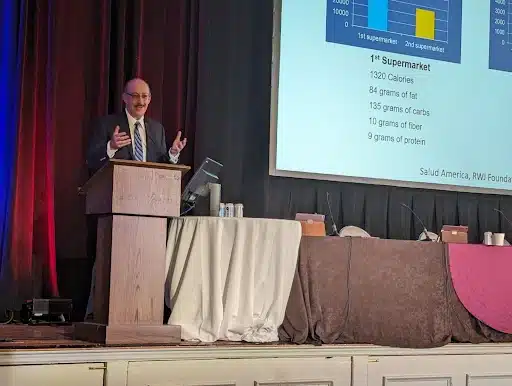
Robert. H. Eckel, MD, began with discussing the evidence for lifestyle interventions on modifiable risk factors for cardiovascular disease and mortality. “Keep in mind,” began Dr. Eckel, “that these are things we measure in almost every patient we see. BMI, systolic blood pressure, non-HDL cholesterol, smoking and diabetes are the five modifiable risk factors examined by The Global Cardiovascular Consortium.”
Dr. Eckel cited results from this publication in the New England Journal of Medicine, which showed that “57.2% and 52.6% of cases of incident CVD among women and men, respectively, and 22.2% and 19.1% of deaths from any cause among women and men, respectively may be attributable to these five modifiable risk factors.”
Keith C. Ferdinand, MD, took the podium next to discuss hypertension, “the risk factor that has the greatest attributable risk of cardiovascular disease in the world.” Dr. Ferdinand lauded the 2023 guidelines released by the European Society Hypertension, which detail management best-practices for arterial hypertension, making note of their decision to “uphold the blood pressure goal of less than 130/80 based on observational and clinical trial data.”




Deepak L. Bhatt, MD, MPH, covered new advances in renal therapies, beginning with the recent EMPA-KIDNEY trial results published in the New England Journal of Medicine. Dr. Bhatt noted that this important trial looked promising for chronic kidney disease (CKD) in patients with and without diabetes. The effects of empagliflozin in patients at risk for disease progression in CKD were promising, although Dr. Bhatt cautioned that “it takes about 18 months to see improved kidney function with any sodium-glucose cotransporter 2 (SGLT2) inhibitor.”
When Anne L. Peters, MD, took her place at the podium to present the latest in diabetes, she joked that all the agents in her field had been consumed by the cardiologists and nephrologists. The only diabetes therapy that hadn’t been taken over for weight loss or CKD was a new cellular therapy for type 1 diabetes, but she conceded it had been shut down by the FDA because of its high cost, risk of side effects, and need for immunosuppression. She then discussed the new Bionic Pancreas insulin pump which uses artificial intelligence (AI) to personalize insulin treatment based on patient body weight and target glucose.
"I can't think of a better statement to share at this meeting than the new American Heart Association's Presidential Advisory on cardiovascular-kidney-metabolic health, which is really why we are all here. The AHA points to different elements of the underlying science like inflammation, oxidative stress, insulin resistance, and vascular dysfunction as underpinnings of this disease state. I encourage everyone to download the document and look at the evidence they provide for lifestyle therapy and medical treatment for the disease from stages 0 to 4."
Dr. Depak L. Bhatt
View the AHA Presidential Statement:
The 2023 Keynote Address: Screening for Social Determinants of Cardiometabolic Health and Practice Implications
"Social determinants of health are the conditions in which people are born, grow, live and work. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels. These social determinants of health are mostly responsible for health inequalities, which are the unfair and avoidable differences in disease incidence between groups."
Dr. A. Enrique Caballero
Diving Deeper Into Exercise Regimens for Cardiometabolic Health
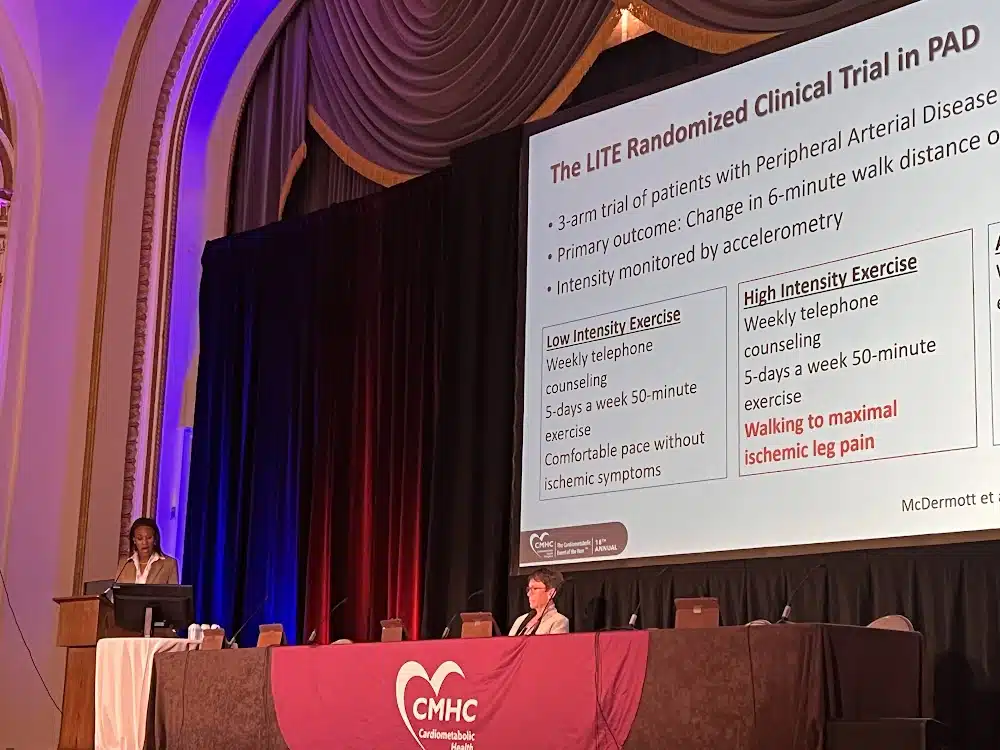
Dr. Eckel introduced his colleagues Jane EB Reusch, MD, and Mercedes Carnethon, PhD, to present the session on exercise as a modifiable lifestyle factor to improve cardiometabolic health. Dr. Carnethon, a behavioral health researcher from Northwestern University Feinberg School of Medicine, made a case for the effectiveness and safety of high intensity, short duration exercise for cardiovascular disease prevention and management in adults. She pointed out that the 2018 Physical Activity Guidelines for Americans emphasizes “a number of alternatives to achieve the activity goals, including 150 minutes per week of moderate-intensity physical activity, 75 minutes of vigorous-intensity activity, or two hours of muscle strengthening activities, offering multiple ways to achieve these recommendations.”
Dr. Reusch then stepped in to address how to achieve physical activity goals in patients with frailty, noting that “decreased exercise capacity is a primary determinant of cardiovascular morbidity and mortality.”
"We need to let patients know that it matters how much you move, and it matters how long you move."
Dr. Jane EB Reusch
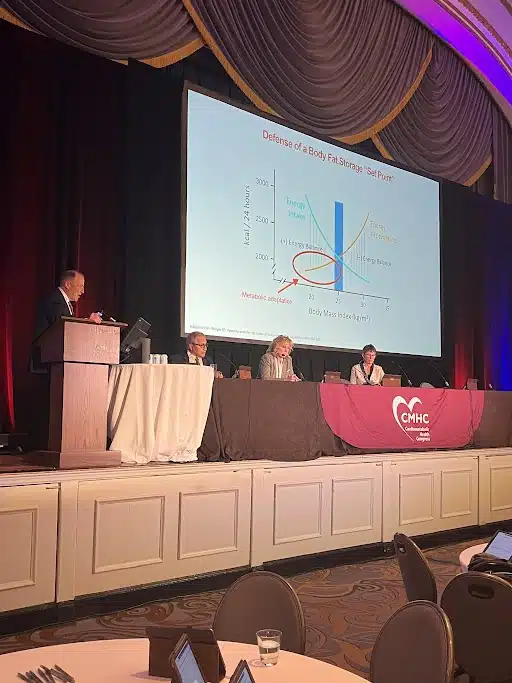
Is it Time to Compare High-Intensity Pharmacotherapy to Surgery for the Management of Obesity?
Moderator Dr. Eckel was pleased to welcome two of his longtime colleagues to engage in an intellectual battle over the future of anti-obesity management. Donna H. Ryan, MD, went on the offensive for the unlimited potential of new pharmacotherapy for obesity treatment, while Christopher D. Still, DO, defended the long-held position that bariatric surgery is the best sustainable solution for weight loss. Both Drs. Ryan and Still ended their compelling arguments with friendly concessions to the others’ points, and Dr. Eckel diplomatically declared the debate a tie.

"Less than 1% of the patients with obesity that meet the criteria for either surgery or pharmacotherapy actually undergo treatment, so there's a huge opportunity not only for pharmacotherapy but for patients to undergo life-extending surgery."
Dr. Christopher D. Still
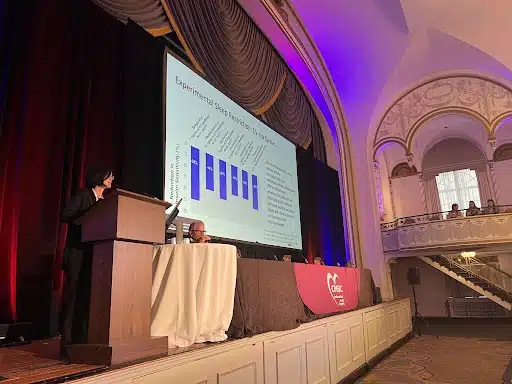
The Intersection of Sleep and Cardiometabolic Risk: Important Connections and Practice Implications
As Dr. Eckel introduced Sirimon Reutrakul, MD, to the stage to present her session on the importance of sleep in patients with cardiometabolic disease, he noted the significance of this topic in light of the 2022 addition of a sleep metric to American Heart Association’s Life’s Essential 8™ . During her presentation, Dr. Reutrakul emphasized that it isn’t just the obvious sleep disorders like sleep apnea and narcolepsy that affect cardiometabolic health. Even slightly restricted sleep in healthy people, between 4 to 6 hours per night, showed a reduction in insulin sensitivity in one study.
The Intersection of MASLD and Cardiometabolic Risk
The session on cardiometabolic disease and hepatic considerations began with an important update to the medical terminology. Long know as nonalcoholic fatty liver disease (NAFLD) and its most serious form, nonalcoholic steatohepatitis (NASH), these conditions have recently undergone a name change at the behest of clinicians and public health experts in the U.S.
Duke University Health System hepatologist Amreen Dinani, MD, MSc, explained that the terms NAFLD and NASH were coined in the 1980s and had been used without much thought since. But in 2022 there was an initiative fueled by the scientific community and patient advocacy boards to update the terminology, removing the potentially stigmatizing mentions of ‘alcohol’ and ‘fat.’ As of June 24, 2023, the newly favored term is metabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH) with an overarching term called steatotic liver disease that refers to any occurrence of fat on the liver.
Dr. Dinani stressed that, while the nomenclature has changed, the pathological definitions have not. There is also a new category that includes liver fat as a result of both metabolic disease and some use of alcohol, which is called metabolic alcohol-associated liver disease (MetALD). The worldwide prevalence of these conditions, characterized by liver inflammation and injury, with or without fibrosis, is on the rise alongside obesity, insulin resistance, dyslipidemia and hypertension.
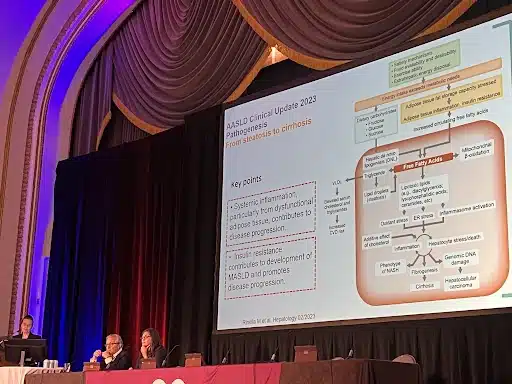
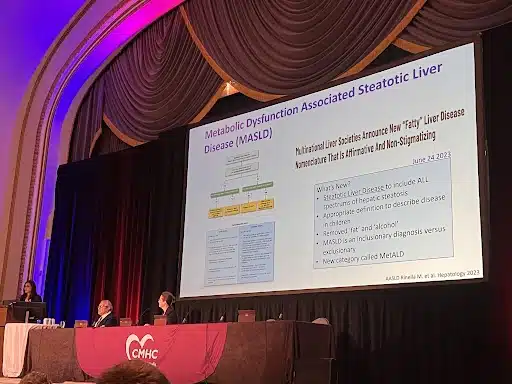
After Dr. Dinani cleared up the terminology, Diana D. Barb, MD, an endocrinologist from the University of Florida College of Medicine, referenced the new American Association for the Study of Liver Diseases (AASLD) 2023 guidance document, which points to metabolic pathogenic drivers of MALFD as key therapeutic targets, with particular focus on systemic inflammation stemming from adiposity and insulin resistance.
The AASLD document notes the “ongoing debate over the nomenclature of fatty liver disease,” had not yet been finalized at the time of publication in May 2023. The authors note that, “it is intended that any formal change in nomenclature will advance the field without a negative impact on disease awareness, clinical trial endpoints, or the drug development/approval process. Furthermore, it should allow for the emergence of newly recognized disease subtypes to address the impact of disease heterogeneity, including the role of alcohol, on disease progression and response to therapy. Input from patients has been central to all stages of the consensus process to ensure the minimization of nomenclature-related stigma.”
View the AASLD guidance:
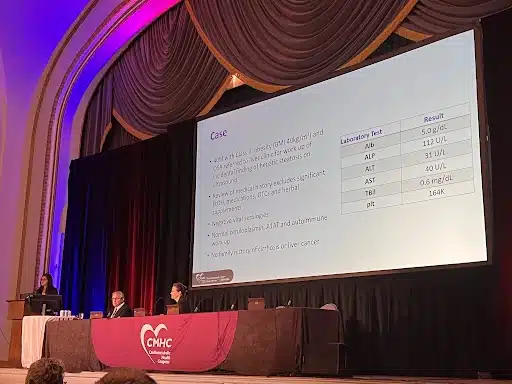
Challenging Obesity Cases and Panel Discussion
Many of the afternoon’s experts returned to the stage for the culmination of the day’s education, when the principles they presented during their lectures are tested against real patient cases. The experts quizzed each other and the audience of providers to see if their treatment decisions matched the ones they made in clinic. These challenging cases are a mainstay of CMHC’s education, as they are a chance to translate the didactic portion of the conference into a relatable clinic experience that attendees could face on Monday morning.
Welcome Reception and Networking
The day’s educational sessions closed with a cocktail hour during which attendees, faculty, and industry representatives mingled and connected. After the networking reception, many audience members enjoyed dinner and cocktails at Off the Common, Boston Park Plaza’s lobby bar, or took a short walk to one of the many eateries in Boston’s trendy Back Bay. Another day of education begins tomorrow morning for the thrid day of the 18th Annual CMHC.