Today marks the third day of the 17th annual conference from Cardiometabolic Health Congress (CMHC). In the past 17 years, this medical conference has grown to be the pinnacle event in evidence-based education for the diagnosis, treatment, and management of cardiometabolic diseases and risk factors. The event is hosted by the Boston Park Plaza, an iconic venue in Boston’s Back Bay. Read on for a recap of the day’s sessions.
Sunrise CME Breakfast Symposium: Navigating the Diagnosis and Treatment of Patients with Narcolepsy and Cardiovascular Risk
7 a.m. EST — The third day of the 17th Annual CMHC began early with a special breakfast symposium. Virend Somers, MD, PhD, from Mayo Clinic in Rochester, Minnesota, Phyllis C. Zee, MD, professor of neurobiology at Northwestern University in Chicago, and Richard K. Bogan, MD, from the University of South Carolina School of Medicine in Charleston, discussed the unique intersection between disordered sleep and cardiometabolic risk.

Read more about The Implications of Sleep Disorders on Cardiometabolic Health
Session II: Dyslipidemia/Atherosclerosis/Thrombosis
8 a.m. EST — Patrick M. Moriarty, MD, professor of medicine and director of clinical pharmacology at the University of Kansas Medical Center, gave audience members a comprehensive overview of the low-density lipoprotein variant, LP(a), that has been identified as a risk factor for atherosclerosis and related diseases such as cardiovascular disease and stroke. In a post hoc analysis of the ODYSSEY OUTCOMES trial, Dr. Moriarty and colleagues determined that lowering LP(a) contributed independently to cardiovascular event reduction, supporting the concept of LP(a) as a treatment target in individuals with recent acute coronary syndrome.

Read a full recap of Dr. Moriarty’s presentation on LP(a) courtesy of our partners at Healio.
Primetime CME Symposium: Escaping the Current Gaps in the Understanding and Treatment of CKD Anemia
9:05 a.m. EST — To kick off the morning’s symposium on the role of iron in chronic kidney disease (CKD), Bradley M. Denker, MD, discussed iron on a chemical level. “Iron deficiency is the first, second, and third reason a patient with CKD will be anemic, but rule out other causes such as thyroid disorders, hemolysis, nutritional causes, or malignancy,” advised Dr. Denker. But, he cautioned, “there is also a downside to iron supplementation; there is a potential for iron overload, and too much can increase the risk of some infections.”

Ajay K. Singh, MBBS, FRCP, MBA, began his session on the treatment of anemia in patients with CKD by polling the audience on whether or not there are any FDA-approved agents for the treatment of anemia in CKD. In fact, no HIF-PH inhibitors are currently approved, but there are four of them in Phase 2 and 3 clinical trials in the U.S. These promising therapeutics improve iron mobilization to the bone marrow and stimulate endogenous erythropoietin production even in patients with end-stage CKD.
“Despite having the evidence, guidelines, and agents to treat anemia in patients with CKD, we aren’t delivering this care to enough patients. The drivers of the high cost of iron supplementation include the price of storing, transporting, and administering IV iron, as well as the fact that people who need iron are probably also receiving blood transfusions.” – Dr. Singh
For more on this topic, visit CMHC’s Iron Deficiency in Chronic Kidney Disease Digital Education Hub
The Changing Treatment Landscape in Dyslipidemia
“I want to remind everyone that atherosclerosis is a systemic disease,” Pam R. Taub, MD, began her lecture, and that although stents and other focused therapies exist, “we really want to address it with systemic agents which we know yield fantastic results.” When statins were developed and approved in the 1980s, they were an iconic class of drugs and remain hugely helpful in lowering LDL-C, but we are experiencing somewhat of a renaissance with PCSK9i agents for lowering lipid levels.

In closing, Dr. Taub remarked that patients identified as good candidates for PCKS9i and other agents aren’t the ones she worries about but that “subclinical atherosclerosis is what keeps me up at night; these patients are ticking time bombs walking around with elevated LDL-C and unaware of it.”

Session III: Diabetes
1:25 p.m. EST — To begin the afternoon sessions on diabetes, Anne L. Peters, MD, welcomed some of her colleagues and fellow experts on diabetes care to the stage. Registered dietician at the University of Washington Medicine Alison B. Evert, RDN, CDCES, said, “As a dietician, I see myself as a coach. My job is to help patients create a nutrition plan, but first, I need to know them. I have a patient from India, and she’s a vegetarian. Knowing this, I can create a plan that’s right for her, and that ultimately she’ll have better luck adhering to.”

Carbohydrate quantity vs. quality in diabetes health is of utmost importance when considering a diet for patients with diabetes. Dr. Evert highlighted four main markers of carbohydrate quality:
- Source. Consider whether the carbohydrate load is coming from processed sugary foods or from better sources such as legumes, fruits, and grains.
- Glycemic index. Studies show that eating a diet low on the glycemic index results in small but meaningful reductions in A1c, fasting glucose, lipids, adiposity, blood pressure, and inflammation in patients with type 2 diabetes. Consider foods higher in carbohydrates but low on the glycemic index.
- Fiber. According to the Dietary Guidelines for Americans 2020-2025, 90% of women and 97% of men do not meet the recommended dietary intake of 14g of fiber per 1000 calories. Consider if the sources of carbohydrates are also fiber-rich foods like whole fruits.
- Sugar. Limiting the intake of sugary beverages like sodas and juices has long been emphasized for carbohydrate reduction, but recent studies also reveal dangerous associations between artificial sweeteners and cardiometabolic health, so water is the best choice for patients with diabetes.
“If a patient wants to follow a low-carbohydrate diet, that’s wonderful, but we find that it’s hard to stick to long term, and when carbs go down, fat tends to go up, and it’s not unsaturated fat. We don’t want our patients with diabetes to die from heart disease, and unfortunately, that’s the leading cause of death in these individuals.” – Dr. Evert
1:45 p.m. EST — In a special session supported by a grant from Dexcom, Irl B. Hirsch, MD, presented some insights and tips for integrating the use of continuous glucose monitors (CGMs) into daily patient care. He remarked that “the data from the RWE 1 trial, investigating the use of CGM showed drastic reductions in acute diabetes-related events and hospitalizations.”
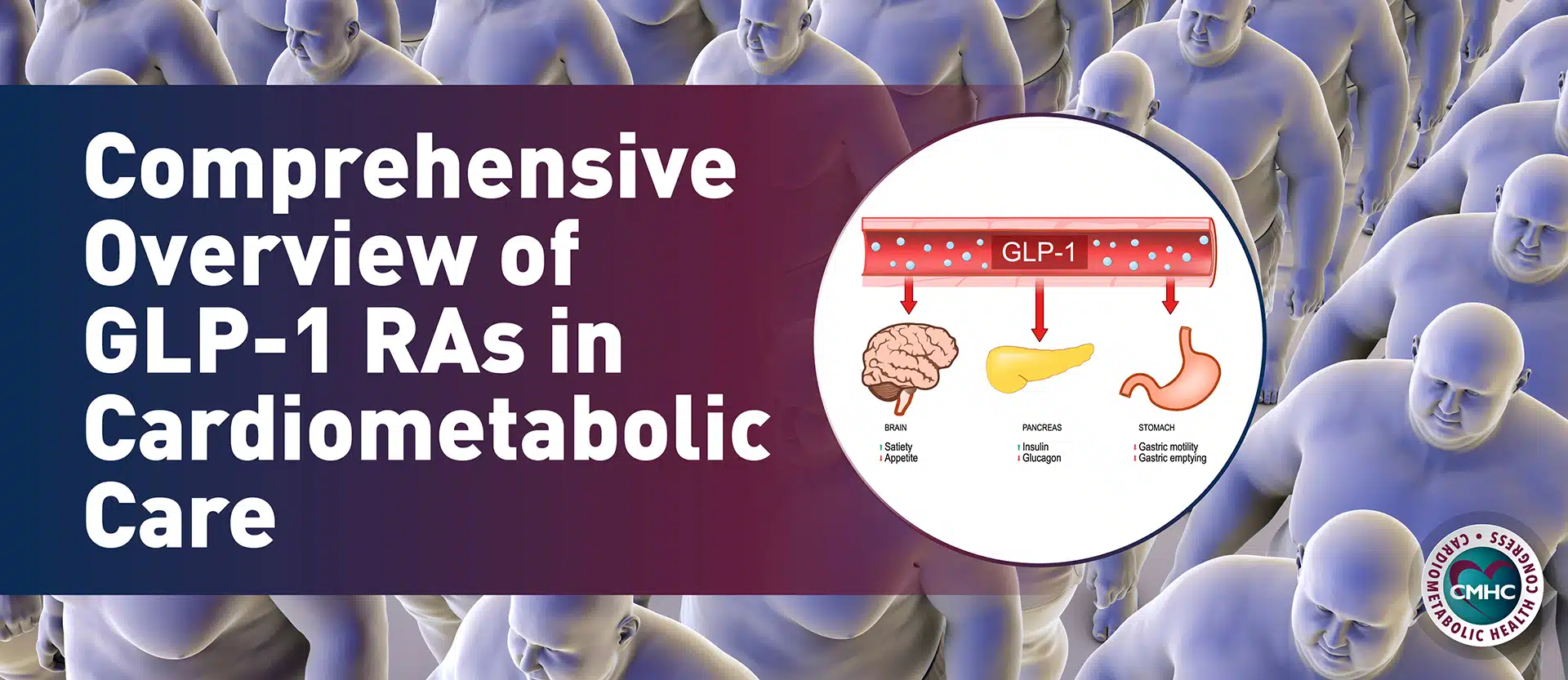
Primetime CME Symposium: Assessing the Evolving Role of GLP1-RAs to Reduce Cardiovascular Risk
2:10 p.m. EST — With support from an educational grant from Novo Nordisk, the Friday afternoon symposium covered emerging evidence, evolving guidance, and expert perspectives regarding the use of GLP1-RAs in cardiovascular risk reduction. Session faculty Marie E. McDonnell, MD, and Jorge Plutzky, MD, discussed several studies that demonstrate the use of these agents can benefit cardiovascular function and kidney health in addition to their original indication for lowering blood glucose in people with diabetes.


“Cost is a side-effect. When thinking about possible deterrents to a patient starting on a course of these agents, you must consider not only the physical symptoms but the out-of-pocket price for the medicine, and if they’ll be willing or able to pay it.” – Dr. McDonnell
3:40 p.m. EST — In his session on Emerging Treatment Options for Diabetes, Juan P. Frias, MD, from the University of California San Diego, explained that some newly approved doses of injectable agents can help patients can reach glycemic control weight-loss goals with higher doses of dulaglutide (3-4.5 mg) and semaglutide (2 mg) when they’d plateaued on the previous maximum dose. Dr. Frias reminded listeners that there are biomechanical and psychosocial effects of obesity in addition to the cardiometabolic factors we’ve been talking about. A benefit of new, emerging, or expanded-label drugs for diabetes is that they’ll provide modest weight loss in addition to controlling blood glucose.
4:20 p.m. EST — All faculty from the diabetes sessions returned to the stage as each presented a challenging diabetes management case from their practice, discussed treatment options and pitfalls, and then fielded questions from the audience.

STAY TUNED!
Tomorrow, Saturday, Oct. 22, we’ll detail the exciting and enlightening topics presented on the final day of the 17th Annual CMHC. And we’ll reveal which three lucky attendees won the amazing Passport to Prizes drawing at the Friday night Happy Hour!