Hundreds of practitioners gathered at the Boston Park Plaza for the annual conference from Cardiometabolic Health Congress (CMHC) on Oct. 19-22, 2022. Founded in 2006, this medical conference has grown to be the biggest and most-anticipated event in evidence-based education for the diagnosis, treatment, and management of cardiometabolic diseases and risk factors.
Day 1 – Wednesday Oct. 19, 2022

Robert H. Eckel, MD, the stage to welcome the audience of providers in primary care, cardiology, endocrinology, obesity medicine, nutrition, lifestyle, nephrology, women’s health, and many more specialties. “I’m theoretically retired, but it’s a pleasure to be here for another year of cardiometabolic health education,” Dr. Eckel began. “When you use your brain for 45 years, it’s not easy to stop.”
The first speaker of the pre-conference, Donald M. Lloyd-Jones, MD, began by inviting attendees to join CMHC and the American Heart Association (AHA) in Chicago next month for a CME Dinner Symposium. In his presentation on Healthy Aging and Cardiometabolic Risk, he remarked, “When we talk about the three M’s of cardiovascular risk, we want them to be Measurable, Monitorable, and Modifiable,” Dr. Lloyd-Jones explained.
He announced that in June of 2022, the AHA had updated their Life’s Simple 7 guidelines to include a new metric of sleep, renaming it Life’s Essential 8.
He went on to discuss compression of morbidity, joking, “We are all going to die. I hope that doesn’t shock anyone. But compression of morbidity means that the ideal way to die is to get sick as close as possible to your date of death. We want to compress that morbidity to, say, the final two months of life, so we aren’t spending as much of our life sick.”

The pre-conference Primetime CME Symposium, Making Sense of LDL-C Combination Therapy in 2022: Strategies and Pearls to Move Beyond Inertia to Improve Patient Outcomes, was chaired by Christie M. Ballantyne, MD.
As Erin D. Michos, MD, began introducing a real patient case to demonstrate how lowering LDL-C can reduce ASCVD risk, she commented that “cumulative low-density lipoprotein cholesterol (LDL-C) can be achieved through favorable genetics, healthy lifestyle, or early intervention. Whichever the reason, we see that lower lifetime risk of ASCVD is demonstrated in people that never cross the threshold into high LDL-C levels, and if you can lower LDL-C, you can reduce risk.” Read a full recap of Dr. Michos’ session, courtesy of our partners at Healio.
The final general session of the day featured Marie E. McDonnell, MD, who shared her insights on Deprescribing in Older Adults with Type 2 Diabetes. She said that by the end of her lecture on this topic near and dear to her, she hoped the audience would not consider this concept DEprescribing, but rather, REprescribing, in which “the practice of categorizing your patients not just by their age – but by their overall health with consideration of cognitive impairment – will help you decide how much preventative potential you have.” She elaborated, “There are complex links we should keep in mind – cognitive impairment is about 70% higher in older adults with diabetes than in their non-diabetic counterparts.”
An Expert Panel Discussion and Audience Q&A closed out the first day of the 17th Annual CMHC, with Dr. Eckel serving as moderator. Many of the day’s presenters joined him onstage to review the day’s topics, which focused on increasing cardiometabolic health and the overall number of healthy years for older adults.
Day 2 – Thursday, Oct. 20, 2022
Opening Remarks, FDA Updates, and Late-Breaking Trials
Opening remarks from chairperson Christie M. Ballantyne, MD, began the morning presentations on late-breaking trials and recent FDA approvals in six key areas of cardiometabolic medicine. “For me, this is one of the most exciting aspects of this meeting. This field has been exploding over the last few years in terms of the impact we can make.”Continue reading for the six therapeutic areas discussed and the CMHC experts who presented the trials, drugs, advances, and setbacks experienced in each field over the year that’s passed since the last CMHC annual conference:
Updates in Hypertension, presented by Keith C. Ferdinand, MD, professor of medicine, and Gerald S. Berenson, Endowed Chair in Preventive Cardiology at Tulane University School of Medicine. In his presentation on new and emerging therapies for managing resistant hypertension, Dr. Ferdinand reminded audience members that “blood pressure is the most powerful and consistent predictor of cardiovascular disease.”

Updates in Obesity Medicine, presented by Robert H. Eckel, MD, professor emeritus, and Charles A. Boettcher II, Endowed Chair in Atherosclerosis at the University of Colorado School of Medicine Anschutz Medical School. Dr. Eckel covered a study investigating the number of optimal steps per day to combat obesity and overweight but noted that results must be adjusted for rate-of-step, as those who walk more slowly may still benefit even if they don’t make the 10,000 steps-per-day marker. He also reviewed impressive data from a recent trial of tirzepatide, remarking the “impressive data in terms of the dose escalation for a 10-15 mg dose resulted in more weight loss, indicating very good results when compared to placebo.”
Updates in Cardiovascular Disease, presented by CMHC Senior Planning Committee member Deepak L. Bhatt, MD. Dr. Bhatt took the podium to discuss the latest trials in cardiovascular disease, summing up a dosing trial results by saying, “The message is that in stable patients, sure, you can get away with shorter-duration therapy, but long-term dual-antiplatelet therapy is still the gold standard for patients at high risk for ACS.”

Updates in Diabetes, presented by Anne L. Peters, MD.”I like things that make my patients happy, and the Freestyle Libre 3 makes my patients happy,” she said regarding the April 2022 approval of the continuous glucose monitor (CGM). “It’s the size of a penny, it goes directly to a patient’s smartphone, and the little tiny disk is less likely to irate the skin. There are a couple of downsides – it’s not approved by Medicare because they don’t consider a smartphone a medical device. This is a problem for my under-resourced patients in terms of affordability.”

Updates in Renal Disease presented by George L. Bakris, MD, opened with the comment, “SGLT-2s are cardiorenal risk-reducing drugs that HAPPEN to lower glucose,” jokingly directed at Dr. Peters, who had just wrapped up her discussion of their use in diabetes management. As principal investigator on the finerenone trial, Dr. Bakris observed markedly slow disease progression in participants using this agent. Regarding an investigation on whether the time of day affects drug efficacy, he said, “There is no credible data to support taking your meds at night. If it’s more convenient, fine, but it’s not going to improve your outcomes.”

Updates in Lipids presented by Christie M. Ballantyne, MD, closed the morning’s sessions on late-breaking trials and FDA approvals. Dr. Ballantyne discussed lipid-lowering therapies in development, saying there had been one new approval since our meeting last year (inclisiran) and a new pathway that came out in August focusing on a novel LDL threshold. “It’s been a tough year for triglycerides. I showed this slide last year, and we’ve already lost two players, but there’s a new player; we are looking into pegozafermin for people with very high triglycerides. This agent has been looked at for liver fat in NAFLD and NASH, as well. I’m looking forward to seeing what this does in Phase II.”

Keynote Address
The Keynote Address was delivered by Louis Philipson, MD, PhD, on therapeutic inertia in Cardiometabolic Disease. He said of the conference, “This is actually my first time here, and I’m in awe of what I’ve learned already this morning.” Read a full recap of Dr. Philipson’s keynote address, courtesy of our partners at Healio.
“Therapeutic inertia is not only the failure of providers to increase pharmacologic therapy when treatment goals are unmet, but includes the broader concept of underutilizing interventions known to prevent negative outcomes.” – Dr. Philipson
Attendees enjoyed a break in the Exhibit Hall, where industry members answered questions, offered solutions, and connected their brand’s products and solutions with CMHC’s provider audiences.

Session I: Obesity & Lifestyle
For the afternoon sessions on obesity and lifestyle, Dr. Eckel returned to give the opening remarks and introduce the expert lineup of speakers to discuss areas of approach to improve outcomes and reduce obesity-associated diseases and risk factors.
Physical Activity & Cardiometabolic Health: Benefits and Perspectives presented by Jill Kanaley, PhD, exercise physiologist and professor at the University of Missouri.

“Exercise increases insulin sensitivity acutely up to 24-48 hours post-exercise, but is not a chronic effect unless patients participate in regular activity at least every other day.” – Dr. Kanaley
Presented by Amy Hess Fischl, MS, RD, LDN, BC-ADM, CDCES, advanced-practice dietitian and diabetes care specialist at the University of Chicago.

“We need to look at the quality of diet. For instance, someone may be vegetarian but consume large quantities of cheese, peanut butter, and processed foods. So, someone who eats meat may very well be consuming more plant-based foods than a vegetarian.” – Dr. Hess-Fischl
Pre-Obesity: Intervening Early to Decrease Future Complications
This lecture was presented by Michelle L. Look, MD, obesity medicine physician at the San Diego Sports Medicine and Family Health Center. Read a full recap of Dr. Look’s presentation, courtesy of our partners at Healio.

Dispelling Common Myths About Obesity
In this energetic and engaging presentation, obesity medicine physician scientist Fatima Cody Stanford, MD, MPH, MPA, MBA, explained why all calories are not created equal, why obesity is a disease, not a bad habit or lack of willpower, and why the most important organ involved in obesity is the brain.

Making Sense of the Evolving Treatment Landscape in Obesity
Louis J. Aronne, MD, professor of metabolic research at Weill Cornell Medicine and director of the Comprehensive Weight Control Center, presented this captivating session complete with a challenging patient case.
In many attendees’ favorite part of the conference, a panel of experts took the stage to discuss some challenging real-life cases in patients with obesity. Featuring lively debate and audience interaction, the experts imparted insights and tips that audience members can implement into patient care right away on Monday morning.

Day 3 – Friday, Oct. 21, 2022
Sunrise CME Breakfast Symposium: Navigating the Diagnosis and Treatment of Patients with Narcolepsy and Cardiovascular Risk
The third day of the 17th Annual CMHC began early with a special breakfast symposium. Virend Somers, MD, PhD, from Mayo Clinic in Rochester, Minnesota, Phyllis C. Zee, MD, professor of neurobiology at Northwestern University in Chicago, and Richard K. Bogan, MD, from the University of South Carolina School of Medicine in Charleston, discussed the unique intersection between disordered sleep and cardiometabolic risk.

Read more about The Implications of Sleep Disorders on Cardiometabolic Health
Session II: Dyslipidemia/Atherosclerosis/Thrombosis
Patrick M. Moriarty, MD, professor of medicine and director of clinical pharmacology at the University of Kansas Medical Center, gave audience members a comprehensive overview of the low-density lipoprotein variant, LP(a), that has been identified as a risk factor for atherosclerosis and related diseases such as cardiovascular disease and stroke. In a post hoc analysis of the ODYSSEY OUTCOMES trial, Dr. Moriarty and colleagues determined that lowering LP(a) contributed independently to cardiovascular event reduction, supporting the concept of LP(a) as a treatment target in individuals with recent acute coronary syndrome.

Read a full recap of Dr. Moriarty’s presentation on LP(a) courtesy of our partners at Healio.
Primetime CME Symposium: Escaping the Current Gaps in the Understanding and Treatment of CKD Anemia
To kick off the morning’s symposium on the role of iron in chronic kidney disease (CKD), Bradley M. Denker, MD, discussed iron on a chemical level. “Iron deficiency is the first, second, and third reason a patient with CKD will be anemic, but rule out other causes such as thyroid disorders, hemolysis, nutritional causes, or malignancy,” advised Dr. Denker. But, he cautioned, “there is also a downside to iron supplementation; there is a potential for iron overload, and too much can increase the risk of some infections.”

Ajay K. Singh, MBBS, FRCP, MBA, began his session on the treatment of anemia in patients with CKD by polling the audience on whether or not there are any FDA-approved agents for the treatment of anemia in CKD. In fact, no HIF-PH inhibitors are currently approved, but there are four of them in Phase 2 and 3 clinical trials in the U.S. These promising therapeutics improve iron mobilization to the bone marrow and stimulate endogenous erythropoietin production even in patients with end-stage CKD.
“Despite having the evidence, guidelines, and agents to treat anemia in patients with CKD, we aren’t delivering this care to enough patients. The drivers of the high cost of iron supplementation include the price of storing, transporting, and administering IV iron, as well as the fact that people who need iron are probably also receiving blood transfusions.” – Dr. Singh
For more on this topic, visit CMHC’s Iron Deficiency in Chronic Kidney Disease Digital Education Hub
The Changing Treatment Landscape in Dyslipidemia
“I want to remind everyone that atherosclerosis is a systemic disease,” Pam R. Taub, MD, began her lecture, and that although stents and other focused therapies exist, “we really want to address it with systemic agents which we know yield fantastic results.” When statins were developed and approved in the 1980s, they were an iconic class of drugs and remain hugely helpful in lowering LDL-C, but we are experiencing somewhat of a renaissance with PCSK9i agents for lowering lipid levels.

In closing, Dr. Taub remarked that patients identified as good candidates for PCKS9 inhibitors and other agents aren’t the ones she worries about but that “subclinical atherosclerosis is what keeps me up at night; these patients are ticking time bombs walking around with elevated LDL-C and unaware of it.”

Session III: Diabetes
To begin the afternoon sessions on diabetes, Anne L. Peters, MD, welcomed some of her colleagues and fellow experts on diabetes care to the stage. Registered dietician at the University of Washington Medicine Alison B. Evert, RDN, CDCES, said, “As a dietician, I see myself as a coach. My job is to help patients create a nutrition plan, but first, I need to know them. I have a patient from India, and she’s a vegetarian. Knowing this, I can create a plan that’s right for her, and that ultimately she’ll have better luck adhering to.” Read a full recap of Evert’s session, courtesy of our partners at Healio.

Carbohydrate quantity vs. quality in diabetes health is of utmost importance when considering a diet for patients with diabetes. Dr. Evert highlighted four main markers of carbohydrate quality:
- Source. Consider whether the carbohydrate load is coming from processed sugary foods or from better sources such as legumes, fruits, and grains.
- Glycemic index. Studies show that eating a diet low on the glycemic index results in small but meaningful reductions in A1c, fasting glucose, lipids, adiposity, blood pressure, and inflammation in patients with type 2 diabetes. Consider foods higher in carbohydrates but low on the glycemic index.
- Fiber. According to the Dietary Guidelines for Americans 2020-2025, 90% of women and 97% of men do not meet the recommended dietary intake of 14g of fiber per 1000 calories. Consider if the sources of carbohydrates are also fiber-rich foods like whole fruits.
- Sugar. Limiting the intake of sugary beverages like sodas and juices has long been emphasized for carbohydrate reduction, but recent studies also reveal dangerous associations between artificial sweeteners and cardiometabolic health, so water is the best choice for patients with diabetes.
“If a patient wants to follow a low-carbohydrate diet, that’s wonderful, but we find that it’s hard to stick to long term, and when carbs go down, fat tends to go up, and it’s not unsaturated fat. We don’t want our patients with diabetes to die from heart disease, and unfortunately, that’s the leading cause of death in these individuals.” – Dr. Evert
In a special session supported by a grant from Dexcom, Irl B. Hirsch, MD, presented some insights and tips for integrating the use of continuous glucose monitors (CGMs) into daily patient care. He remarked that “the data from the RWE 1 trial, investigating the use of CGM showed drastic reductions in acute diabetes-related events and hospitalizations.”
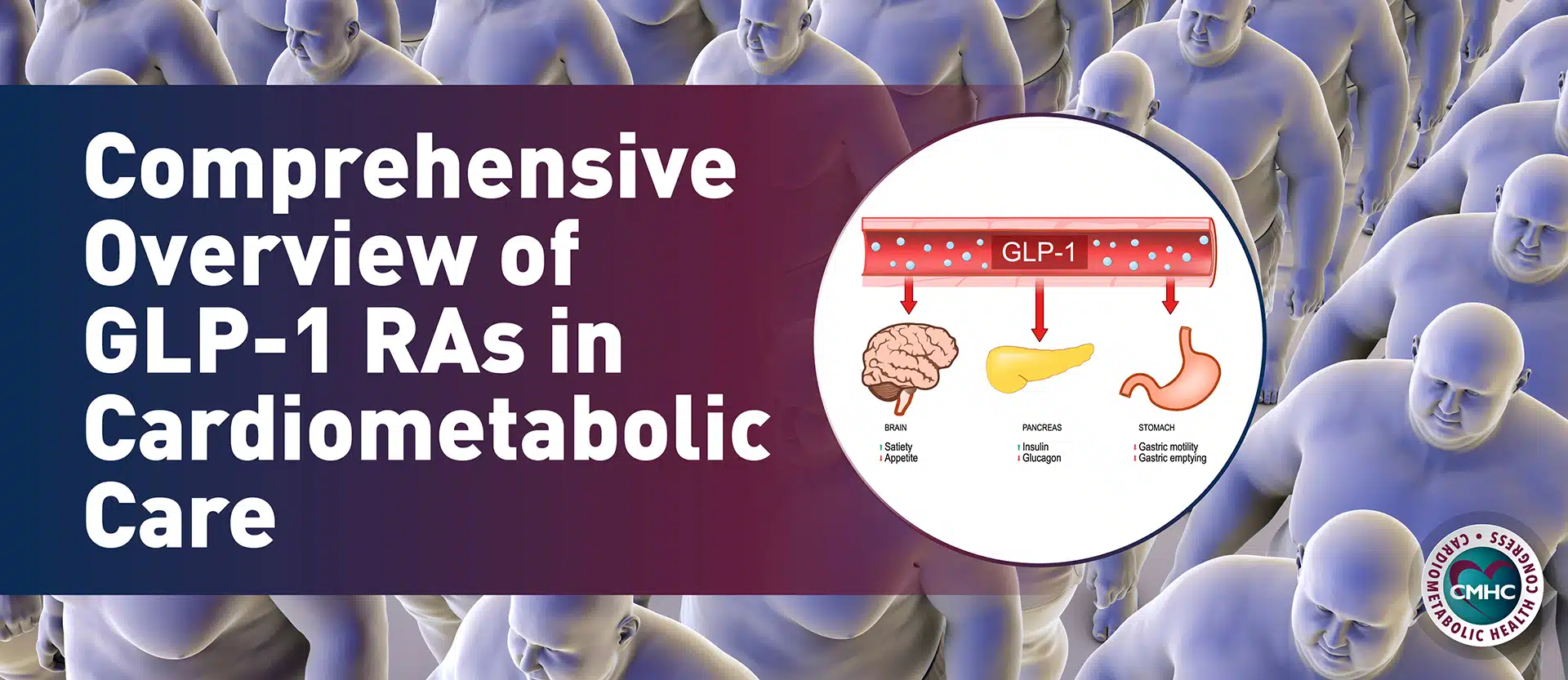
Primetime CME Symposium: Assessing the Evolving Role of GLP1-RAs to Reduce Cardiovascular Risk
With support from an educational grant from Novo Nordisk, the Friday afternoon symposium covered emerging evidence, evolving guidance, and expert perspectives regarding the use of GLP1-RAs in cardiovascular risk reduction. Session faculty Marie E. McDonnell, MD, and Jorge Plutzky, MD, discussed several studies that demonstrate the use of these agents can benefit cardiovascular function and kidney health in addition to their original indication for lowering blood glucose in people with diabetes.


“Cost is a side-effect. When thinking about possible deterrents to a patient starting on a course of these agents, you must consider not only the physical symptoms but the out-of-pocket price for the medicine, and if they’ll be willing or able to pay it.” – Dr. McDonnell
In his session on Emerging Treatment Options for Diabetes, Juan P. Frias, MD, from the University of California San Diego, explained that some newly approved doses of injectable agents can help patients can reach glycemic control weight-loss goals with higher doses of dulaglutide (3-4.5 mg) and semaglutide (2 mg) when they’d plateaued on the previous maximum dose. Dr. Frias reminded listeners that there are biomechanical and psychosocial effects of obesity in addition to the cardiometabolic factors we’ve been talking about. A benefit of new, emerging, or expanded-label drugs for diabetes is that they’ll provide modest weight loss in addition to controlling blood glucose.
Next, all faculty from the diabetes sessions returned to the stage as each presented a challenging diabetes management case from their practice, discussed treatment options and pitfalls, and then fielded questions from the audience.

Day 4 – Saturday, Oct. 22, 2022
Sunrise CME Breakfast Symposium: Navigating the Diagnosis and Management of Heart Failure in Women
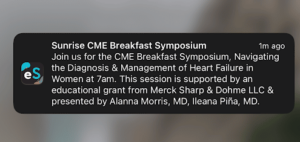
As the final day of of the 17th Annual CMHC began, any attendees who may have tempted to oversleep were reminded via notification from the event’s mobile app (powered by eventScribe) that the sessions were about to commence. Ileana L. Piña, MD, MPH, and Alanna B. Morris, MD, MSc, led the Breakfast CME Symposium on important considerations in managing a spectrum of cardiovascular conditions in women. Dr. Piña, cardiovascular researcher, clinician, and professor of medicine at Thomas Jefferson University, discussed the concept of frailty in her female patients with cardiovascular decline. She noted that light weights and resistance bands can be used to build strength, but only after balance is established in order avoid falls. Not only does decreasing frailty improve physical health, but the psychosocial impacts of regaining independence through improved mobility are significant and contribute to better overall outcomes in women. Read a full recap of Dr. Morris’ session, courtesy of our partners at Healio.
“Frailty is one of those things that is easy to recognize but hard to define.” – Dr. Piña</span
Primetime CME Symposium: The Disproportionate Burden of Atrial Fibrillation in High-Risk African American Patients with Cardiometabolic Comorbidities
After Keith C. Ferdinand MD, introduced the faculty and topic for the morning’s symposium, Duke University Medical Center’s Larry R. Jackson II, MD, reminded the audience that all irregular heartbeats are not atrial fibrillation (A-fib), but that even minutes of true A-fib can lead to stroke weeks later; clinicians must accurately diagnose it and counselling patients on both risks and benefits of anticoagulation therapy. When Dr. Jackson posed the question to fellow faculty member Laura C. Ross, PA-C, regarding whether or not to initiate anticoagulation therapy in patients with A-fib, she said that in her experience “patients are much more scared of having a stroke than a bleed, so I keep that in mind when considering anticoagulation therapy.” Drs. Ross, Ferdinand, and Jackson had a lively discussion on the use of Warfarin versus DOACs; due to their efficacy, consistent dosing, reduced monitoring, fewer drug interactions and generally lower rate of adverse effects, Drs. Ferdinand and Ross were firmly in favor of DOACs, but Dr. Jackson cautioned that the affordability and adherence rates of Warfarin should be considered before completely ruling out its use.
In terms of extended remote monitoring, Dr. Ferdinand commented that newer technology to replace the Holter monitor benefits patients with transportation, time, or care delivery barriers. Dr. Laura Ross agreed, saying that in her clinic they don’t use Holters anymore either, and that “for patients with social determinants of health, newer remote-monitoring devices that look like a bandaid are easier methods we can mail to the patient, they wear it, and mail it back.”
“Encourage clinicians with patients that are non-native English speakers to use the tools at their disposal. Plug your notes into Google translate, it’s free, quick and patients are much more likely to take their medications if they understand why and how to take them, and if they are warned about possible side-effects so they aren’t taken by surprise.” – Dr. Ross
For more on racial disparities in cardiometabolic disease, please listen to Dr. Ferdinand’s award-winning webinar, Looming Cardiometabolic Crisis: A Conversation About Race
Nonsteroidal MRAs: DKD and Beyond

Indiana School of Medicine’s Rajiv Agarwal, MD, MS, discussed the deliberate discovery and ongoing development nonsteroidal mineralocorticoid receptor antagonists (MRAs) to address the need for safer treatments that protect the kidney and heart in patients with diabetic kidney disease (DKD). There are several drugs within this class at varying stages of clinical development, but one of the only approved nonsteroidal MRAs, finerenone, has beneficial renal and cardiovascular properties. Dr. Agarwal posed the question, “What’s wrong with steroidal MRAs like spironolactone?” He explained that spironolactone reduces mortality but is underprescribed due to the perceived risk of hyperkalemia and hormonal side effects. Although the blood pressure reduction with finerenone is less significant, so is the risk of hyperkalemia, according to the FIDELITY-TRH study. Read a full recap of Dr. Agarwal’s session, courtesy of our partners at Healio.
Finerenone is THE drug for the patient shared by the cardiologist and the nephrologist. – Dr. Agarwal
Importance of Assessment and Potential Treatment for Masked Hypertension
For the purpose of his lecture, Raymond R. Townsend, MD presented a working definition of masked hypertension as normal blood pressure (BP) in office, but elevated BP outside of the office. There are a number of potential confounding factors in managing masked hypertension, such as the definition of “normal,” the incidence of occasional high BP in normotensive individuals, and the phenomenon of “white coat syndrome,” which is essentially the opposite of masked hypertension – high BP in the office but normal BP out-of-office. Dr. Townsend discussed masked hypertension findings in studies of three patient populations, concluding that masked hypertension is more prevalent than previously estimated, particularly episodes of asleep hypertension which has serious cardiovascular implications. Read a full recap of Dr. Townsend’s session, courtesy of our partners at Healio.
Challenging Cardiorenal Cases & Expert Panel Discussion
Many of Friday’s faculty returned to the stage to discuss challenging diabetes management case from their practice, discussed treatment options and pitfalls, and then fielded questions from the audience.

THANK YOU to all of our attendees, faculty, exhibitors, and staff that made the 17th Annual CMHC such a wonderful success! Register for next year’s 18th Annual CMHC now for a reduced registration fee!